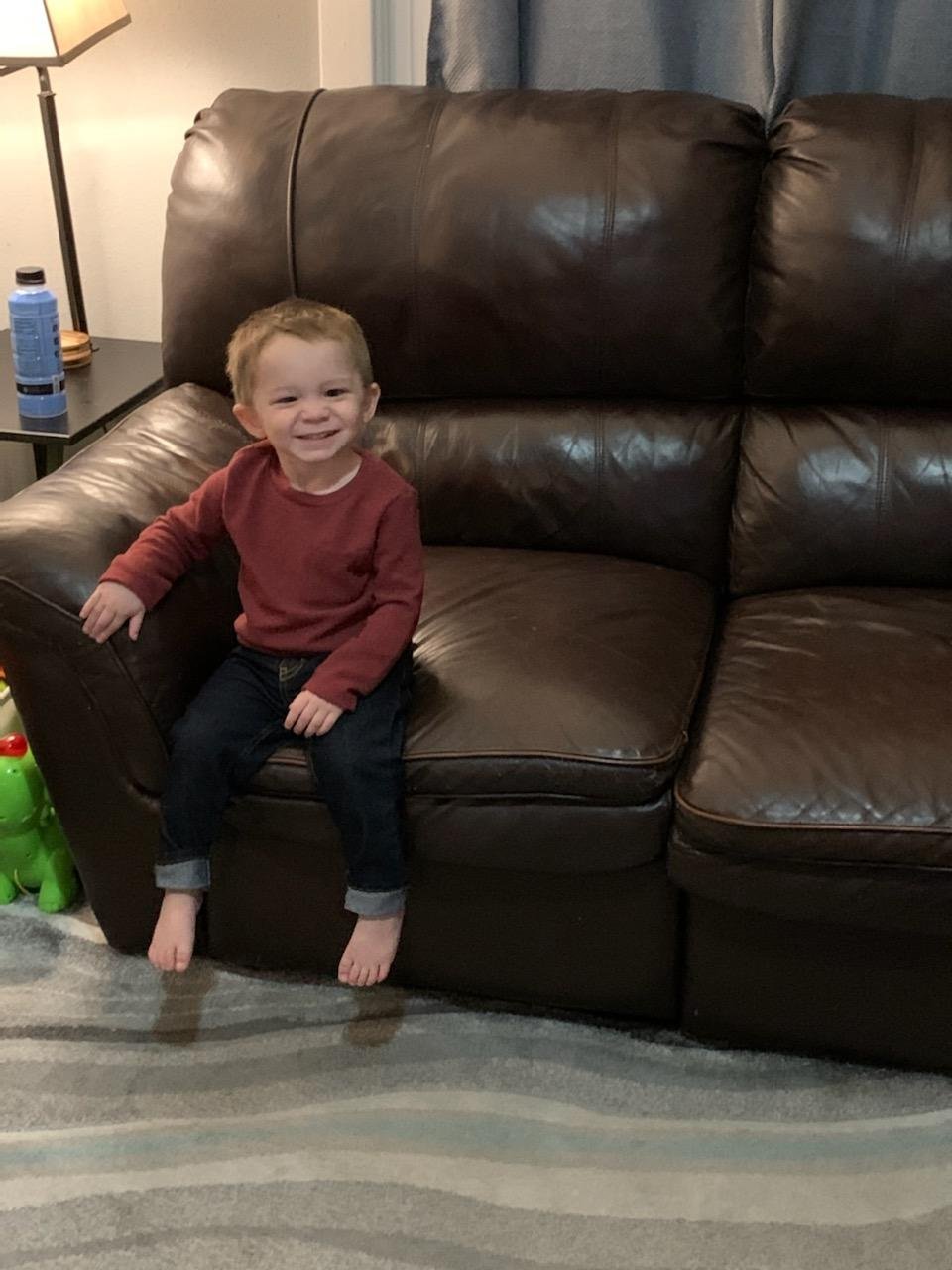
Hudson Smith - Spokane, WA
September 2022
Welcome to our very first newsletter. First off, thank you to everyone who signed up. Also, a very special thank you to all those who donated as without you we would not be able to do this. It is essential that we not only raise awareness about childhood cancer but that we also help share as many stories as we can. The journey through this is not easy and so much is not seen by the general public. Every month we will feature a child going through cancer treatment and give them and their family a voice. We hope that sharing can bring a smile to the families and possibly make their journey a bit easier. We also hope that more awareness will bring more support to other families we cannot directly help.
Without further delay, I would like to introduce everyone to Hudson Smith from Spokane, WA. Hudson just had his third birthday! We hope that he has a great one! Hudson has been fighting Group 3 Medulloblastoma since November 2020 and has faced many challenges along the way. We will let Hudson’s mother, Christina Warrington, tell their story.
Hudson was born September 8th, 2019, on a Sunday. He had a rough start and had to be taken to the NICU because the cord was around his neck twice. Thanks to the angels above and God's love he did just fine. He was a typical developing baby after that, but little did we know he had a storm brewing in his tiny brain. Shortly after his first birthday in October, we took him to an event at his brother's school. Everyone wanted to see how good he could walk (he was becoming really good at walking) so we put him down to show them, and he just stood still and started screaming. We did not think anything of it because there were a lot of new faces around, and we thought he was just scared. Little did we know he was starting a rapid downward spiral. Later that day at home he still refused to walk independently but he would stand and hold onto the couch walking along that. We were concerned but thought he was just worked up after the day's events and will come back to his normal self. The next day was the same thing, not walking and reverting back to crawling. Because he could crawl incredibly fast we assumed it might be stage fright. By the following day he was a little worse, getting upset when standing without holding on to anything and becoming a bit tense. After the weekend was over, we took him to the doctors, and they said it was synovitis in his hip joints (inflammation) from a cold virus but not Covid. They said he would get better in a week or two. We felt relieved that everything was fine. However, he did not get better but instead worse. A week later he was becoming shaky and very slow at his movements and starting to not walk along the couch as much. I took him back in again, and they again felt it was still from a cold virus. They insisted it’s quite common. Over the next few days, he got worse to where he was just lying on the ground shaking. He would try to get up but was moving really slow and having ataxia movements but because he is a baby and was on the ground trying to crawl it was hard to realize he was off balance. He would just slowly lay himself down when playing with toys or trying to crawl/hold himself up. He was not sleeping well but exhausted. We took him in again and we were told they were referring him to pediatric neurology on an urgent referral and the doctor thought it was not synovitis at all but rather Spinal muscular atrophy. We were devastated, the next day I called the neurologist office but was told the doctors reviewed the referral and felt he did not need to be seen urgently and he was ok to wait 3 months for the next opening. I couldn’t handle that response, so I called the nurse at the neurologist office. After waiting and calling multiple times a day I called the pediatrician back and asked for him to help speed this up, get him in for an EEG asap or something or at least call the ER to give them a heads up. Luckily the next day the neurologist office called and said they could do an EEG and meet with us after.
When we went to the neurologist, he felt like it was not spinal muscular atrophy but instead the original diagnosis of ataxia from a cold virus, but he would get an MRI to be safe. To settle our fear, he would ask for the MRI to be ordered as urgent. This never happened over the course of several days. I called and called to pester them. By this time Hudson could not even hold his head up while being held and needed blankets wrapped around him just to hold him up in a reclined highchair seat, choking, vomiting, red and rashy, having temperature regulation problems and not eating or even crying much. We were about ready to drive to Seattle Children’s Hospital ER when I got the hospital at sacred heart to agree to let us self-pay for the MRI (insurance paid this later).
The next morning after a month of watching our sweetheart decline rapidly and begging God every day to please heal our son, let him walk again at the very least just be able to play with a toy and crawl again, we had his MRI. Hudson’s time in the scanner seemed to be taking a long time and was strange. The radiology tech kept coming to the waiting room to tell us he was doing fine and should be done soon but he was out of breath and had a trembling voice and was sweating when talking to us. Once we were in post op with Hudson after his scan the nurse told us they needed to make sure all the images were good before we could leave. This seemed odd and we asked if they didn’t get great quality images, the nurse said they did, they are just making sure everything is fine. The nurses kept whispering with each other and asking if he was being admitted (talking loudly across the room asking “is this one being admitted”) our nurse replied yes just waiting on orders. I replied what is going on and she said I don’t know I just know we were told to not let you leave, and Hudson has a medical hold on him so that he could not leave. We were then told we were being put into a private room. We were moved back to a pre op room where they shut the door and curtains and said Hudson could have a bottle. For 2 and a half hours we sat and waited while no one came in. Finally, a nurse came in with the phone and handed it to me saying the radiologist wants to talk to you. I was scared as scared could be. He told me Hudson has a very large mass in his cerebellum, but the more pressing issue is it is blocking off his entire 4th ventricle and his brain was incredibly compressed against the skull. He said we would be walked down to the ED and the neurosurgeon was going to come meet us and he would have surgery that same day. I was in disbelief and could not control my tears, I remember begging the radiologist to tell me what to do, meanwhile Derek is asking me tell him what’s going on. I was shaking and confused as I told my husband what was happening as he sat there holding our little boy. He held our son tight and started to cry and he mumbled no over and over. I will never forget those few minutes of us hearing the news. The chaplain came in right away and comforted us and walked with us as they took us down to the ER with me carrying Hudson. As I walked, I remember feeling exhausted as if we had walked several miles to get down the hallway. I remember stepping out when we got to the room to go update my close friend who was watching our other son. She immediately offered to keep him for us, and I was so relieved.
When I got back to the room everything went so fast several nurses and techs were in the room to start IVs and fluids and get labs, and all I saw when I walked in was my baby screaming and crying while being held down to start an IV. Shortly after they took us back to pre op and we waited for our oldest son to come to the hospital. This was during Covid when no children or visitors were allowed but due to the circumstances, they made an exception as we found out later that they didn’t think Hudson would make it. I remember feeling so sad for our older son who was confused about what was going on and sad he was not going to be spending thanksgiving with his family or coming home that night. Roman was scared for his brother and was trying so hard to be brave at 9 years old. Not long after Roman came to visit, the priest from our church came to baptize Hudson because the nurses said it was important that he be baptized before the surgery. Little did I know Hudson was starting to die on us, so they took him to surgery earlier than planned. Derek and I walked down the hall to the OR, and I still remember the look on his face as I held him in my arms, crying so hard and begging God the entire way. The look on his face and in his eyes, it was like he knew he was going to be getting help but wanted me to promise him nothing would hurt him. We gave him a kiss goodbye and passed him off. We felt relief when we got the call that the surgeon made the first cut and Hudson was doing ok. We waited anxiously for several more hours, it was nearly 11 pm by the time the surgeon came to talk to us, he told us everything went well and Hudson was in the PICU and would need to stay on the ventilator for the night but was doing good. He explained that Hudson’s intracranial pressure was so high from the hydrocephalus that spinal fluid shot up to the ceiling when he made the first drill hole in his little skull. He said he’s never seen pressure so high.
We were originally told by him that they felt the tumor was a different type then it was. We felt relieved because the original thought was a less aggressive tumor. The surgeon told us we were lucky Hudson was diagnosed when he was because we would have put him to sleep in his crib at home and he would have not woken up and we would have never known why and probably would have never received an answer. We could not believe what we were hearing that our little baby was so close to death that he would have died that night, we couldn’t stop thanking God and his guardian angels for protecting and saving our son.
After we were taken to the PICU, we had to wait almost 45 mins in the hallway before they allowed us to enter the unit while they got him situated. Finally, we got to see our baby. I have worked in the medical field and seen a lot of patients in the ICU, but nothing prepares you for when it’s your own child and even worse your tiny baby. Derek has never seen all the life sustaining equipment before so for him he was even more shocked and confused. For him, he didn’t know what machine did what and how. For me, I just needed to know the numbers so I knew if he was doing any of his breathing on his own. I remember feeling like I could take a breath when I saw he was doing most of the breathing for himself but panicking when they said they were going to keep him asleep for the night so he couldn’t take out the tube. It gave me just a tiny bit of comfort knowing he was fighting the meds to try and wake up. We sat there holding his foot because he had so many IVs there was no hand to hold, trying to take it all in and having the emotions from the day going through our minds and crying and trying to process the fact that our baby was in this position. All in one day, we learned that our baby had cancer, major brain issues, a major surgery, and that he almost died. We almost didn’t get the scan to save him. In the PICU on every fluid and IV med under the sun and on a ventilator, he looked so swollen and beat up. Being away from our other son, desperately wanting to hold our baby, and fear of not knowing what the next days, weeks, months would look like weighed heavily on us.
We were exhausted, and we felt uncomfortable because it was silent. The nurses and doctors just stood there looking at us quietly so we didn’t ask very many questions. The doctor told us we needed to go home and get a few hours of sleep, we didn’t want to leave him. We gave him a long kiss goodbye and whispered to Hudson we promised we would be back in just a few hours. We reluctantly left after asking the staff to promise to call us for anything and everything. We got home after 2 am and planned to wake up at 5 am to go back a little less than 3 hours of sleep was our plan. We laid in bed holding each other crying and I just kept saying I’m so scared. After a few hours at home and an hour of sleep we quickly gathered some of his favorite things and rushed back to the hospital. Once we arrived, we waited just staring at him to come off the ventilator. Finally, 10am came, and they started the process. He did wonderful. He whimpered and reached for us. By noon we had him in our arms. It was the most wonderful feeling like holding him for the first time when he was born but better and more emotional. We spent the next 10 days in the PICU, each night having to leave him. It was so heartbreaking seeing his little cross eyes watch us leave. Each night we would leave one of my shirts with him so he could smell my scent and have some comfort. A couple of days before being transferred from the PICU to oncology, the oncologist came and talked to us to let us know that his tumor was not what they originally thought but was instead medulloblastoma. We didn’t quite know how to process everything and didn’t have all the details yet of just how severe this cancer was. We were told it only takes a couple of months for it to grow from cells to the size it was as it is a very aggressive tumor. We were told that sub typing would take a few weeks and that would determine his treatment plan. However, we went into it thinking it would not be too terribly long that he would be in treatment as we were told it was 7 months. We were so numb we couldn’t ask any questions on prognosis.
The day finally came to transfer to pediatric oncology. We hated it and just wanted to take him home. We were told one day but we ended up having to stay several more days. The doctor made an exception and allowed us to take Hudson to the waiting room to see Roman through the window. Finally, after receiving chemo education of what to do and not to do we were able to come home for a few days before starting treatment. The doctor suggested we do an early Christmas just in case he didn’t get to be released from the hospital. We spent that week at home letting Hudson see his grandparents. We opened presents early and had a small Christmas meal. We saved a lot of presents for Christmas just in case and I’m glad we did because Hudson was able to come home after treatment the day before Christmas Eve.
Two days before chemo started, we received the call we did not want from oncology. His subtype of his tumor was officially large cell anaplastic group 3 medulloblastoma high risk with metastatic disease to his spine. We were told adding a specific chemo would greatly increase his chances of no recurrence and that he would do a specific study after treatments to remove residual tumor. We ended up not needing this as there was no residual tumor. We were devastated, one of the worst subtypes to have is group 3, but because he didn’t have specific amplification of specific proteins in his tumor his chances were a bit better.
There were a lot of chemos. We were released from the hospital to spend Christmas at home. We thanked God because that’s all that was important to be together with our oldest son at home. A few days after treatment Hudson was admitted for neutropenia. He had high fevers, no white cells meaning no immunity, and was very sick. We did this pattern of chemo week in the hospital followed by a week at home and a week to two weeks in the hospital for being septic for almost 8 months. Hudson received 3 cycles of consolidation chemo followed by 3 cycles of high dose chemo with 3 rounds of stem cell rescue. He got to the point where he was so sick that he couldn’t eat and so we had to feed him liquid nutrients through an IV called TPN. We had to continue IV antibiotics and antifungal IVs at home ourselves, injections to boost his cells and nearly 30 meds by feeding tube (NG) in the nose at one point. We even added all night feeds of feeding tube formula through the NG tube at one point. I remember feeling like a self-made ambulance when we would go to Seattle for appointments because we had to run two different iv pumps and feeding tube pump at the same time so I would hang the bags on the hook of the door so we could keep driving while running his meds. He had so many medicines that we would just take the entire bin with us. We had to flush his chest IV several times a day with saline and heparin. His chest IV was called a Hickman line; it was basically two IVs in his chest that went to his heart instead of a port. We also had to change the dressing on this and the caps ourselves. We had to be completely sterile doing it which is a challenge with a baby so we had to wrap him up tight so he wouldn’t move. It was terrible watching our baby scream in pain and for help.
We had a few setbacks during those 8 months. The biggest was subdural bleeding because of the enlarged ventricles. The chemo lowering his platelets made it worse. Hudson had another brain surgery to place a drain tube for a few days and then back to the OR for a subdural drain. He then had two shunts in his head and will have them the rest of his life. He had to have another surgery to replace his Hickman line as it had holes in it. Our baby’s first haircut was done in the OR during his surgery. We were handed his hair in a zip lock bag with a first haircut certificate. Hudson wouldn’t sleep in a crib in the hospital so Derek held him all night long every night in a recliner chair so he could sleep. He did this for 8 months, and it continued at home. He would sleep with him on his chest all night. This continued until just recently, but he still sleeps in our bed because he is scared. What can you expect from a baby who grew up in a hospital? He never received a good night sleep in the hospital being woken up multiple times a night for meds or vital checks, the pain and feeling sick. At one point he was on adult doses of IV morphine through a pain pump.
The high dose chemo rounds were horrible, every 3 hours for 3 days straight being woken up for a bath because the chemo would exit through his sweat and would burn his skin. We were finally able to breathe a sigh of relief when chemo was done, and he had no signs of disease. We were able to let him ring that bell. However, it was Covid, and the hospital was not allowing the end of chemo bell ringing, but it was a Sunday when no one was there to stop him, so they let him do it anyway. We had a drive by end of the chemo celebration parade planned and other than family and a couple of close friends no one showed up. Those who were there were a part of our bell ceremony. We had one close friend drive by and a fire truck other than that he sat in his little wagon waiting for a parade that never happened.
Aside from being heartbroken and feeling let down we were so happy to get back to real life. Unfortunately, after 3 months when we went for our follow up scans in Seattle, we learned his cancer was back. We were given our options of try a different lower dose chemo that would try to hold him off until he’s old enough for radiation or put him on hospice. We were scared to do more chemo but they assured us he would not get sick like before, so we decided to have a port placed and start chemo. This was 5 days in a row of IV chemo. He did not do well with it. It did not drop his white blood counts as low as we expected, but it made him feel very sick. We struggled to get pain meds and nausea meds into him as he hated the feeding tube, but after two rounds we had to use the feeding tube. This went somewhat smooth with a few setbacks, but eventually we were able to keep it in and switch to all oral chemos except one 30 min infusion. He did much better for a while.
After 2 months of treatment, we had another scan in January of 2022 and learned the tumors were still growing. He needed chemo directly to the brain. He had another surgery to place another port into his brain and would continue the other chemos. We again were given the option of hospice, but we would not accept this. We were so glad we made the choice to do intrathecal methotrexate as it actually decreased the tumor size which was not expected. However, getting his brain tapped every 2 weeks under sedation was starting to wear on him.
He was starting to have encephalopathy from neuro toxicity so he was put on robitussin. This was a very tough time as neurotoxicity caused him to have severe rage resulting in him banging his head on the floor repeatedly because the headaches were so severe. He couldn’t understand what was happening. He would bite and scream “ouchi ouchi mommy help me” while clawing at his head. Luckily the robitussin worked, and he started having an easier time with the methotrexate. Hudson had his doses of his other chemos decreased a couple of times due to platelet counts and tolerability. We have just finished his final round of chemo on august 21st 2022. He had his final methotrexate in the brain on the 23rd and will have his final 30 min infusion on the 31st of august. He has been struggling during chemo recovery again by not feeling well but his counts have stayed up. We cross our fingers that he won’t need platelets again. Every time his platelets drop below a certain number he needs a CT scan to be sure his bleeding in the brain has not become worse.
September 7th, we will drive from Spokane to Seattle for his MRI and we pray that he does not have tumor progression. On his birthday September 8th, he will have radiation mapping. If he progresses, we stay and do radiation right away. If he does not, he will come home until the 19th when we start radiation at that point. 6 weeks of being put to sleep 5 days in a row for full craniospinal radiation, but this is what needs to be done to keep our baby.
So that’s Hudson’s cancer story. It has not been easy it has been a lot of ups and downs no time for anything but cancer. A lot of days all we could do was lay on the couch with him because he was so clingy and sick. Dishes would go unwashed, laundry unfolded, toys scattered everywhere, items misplaced, late for appointments, juggling two kids who have two very different schedules and must be at two different places at the same time has been a struggle. Because Derek works long hours, I spent most of my time this second diagnosis doing my days alone with both kids, 8-hour days in clinic some days then rushing off to get my other child from school or wherever. Having no one to talk to, feeling like I’m drowning and by the end of the day when Hudson goes to sleep I still can’t always get things done because I am so emotionally overwhelmed and physically exhausted that I just need to sleep. Some days he refuses to fall asleep without us, so I have to go to bed with him even if I have energy to keep going. Derek is stressed everyday having to be away from Hudson during the day to work and not able to help during the day.
The fear of his future is real every day every second and it’s a struggle to try and experience somewhat of a normal life. Both Derek and I as well as Roman have felt very alone throughout this horrible walk just in different ways and some the same. Hudson is always afraid we are leaving him, but the best thing is we all have each other, and we have built some beautiful memories out of a sad situation. We are also so grateful for all the support we have received from all over the past 2 years, the weekly food, clothes and diapers from the grandparents to the hospital, the connections of new friends all these things have helped us get through. It is crazy and yet sad to think that Hudson has had cancer in his little body his entire life. It is an embryonal tumor meaning it was in him from the beginning as cancer cells that were activating to grow. He has had cancer every birthday and we pray that next year for his 4th birthday he truly is in remission. We pray he makes that 5-year survival rate and surpass it putting him in the cured category.
Childhood cancer is anything but a normal life and with a baby who has cancer it is a whole different ball game. I pray that no parent ever has to experience this. Unfortunately, that is not reality as so many do. Each diagnosis is unique, and each journey so different.
Since we received the story from Christina, Hudson had his MRI. The news was good in that his tumors were smaller. Hudson will tentatively start radiation at Seattle Children’s on September 22nd.
If you would like to follow along with Hudson’s journey, he has a Facebook group.
https://www.facebook.com/groups/958874898841898/
Hudson’s family has also set up a GoFundMe account to help with expenses.
https://www.gofundme.com/f/wuhnq-hudsons-fight
There is a new parade for him in the works. If you live near Spokane, WA and would like to participate, please contact either Cody Huber, hubercody@yahoo.com or (509) 954-5777, or Brett Powell, (916) 844-5933. A definitive date has not been set but should occur in late October or November. As we receive more information, we will post it here.
Each month we will spotlight a new family as we have done here. The parents will fill out a questionnaire that will help us pick out items so that we can send them a care package tailored to them. The package will be sent prior to the newsletter. No two families will receive the exact same items as no two families are the same. If you have a child three or younger currently going through cancer treatment and would like to be featured, please submit your information at
Updates…
Hudson started his radiotherapy this past week. We are also happy to report that he received his care package. His favorite animal is a white call duck. The stuffie we found for him was a hit! We wish Hudson well through this part of his journey and will keep everyone updated as he progresses.
At the beginning of November 2022, Hudson finished his radiation and is currently awaiting scans.
Hudson had scans on December 30th. No new spots were found. He did have some changes near his shunt, but those will just be watched for now as they could be attributed to his radiation.
October 2022 - Kehlani Hoke